OCD affects men and women equally. It is also a common condition, affecting about 1 in 40 adults in the United States.
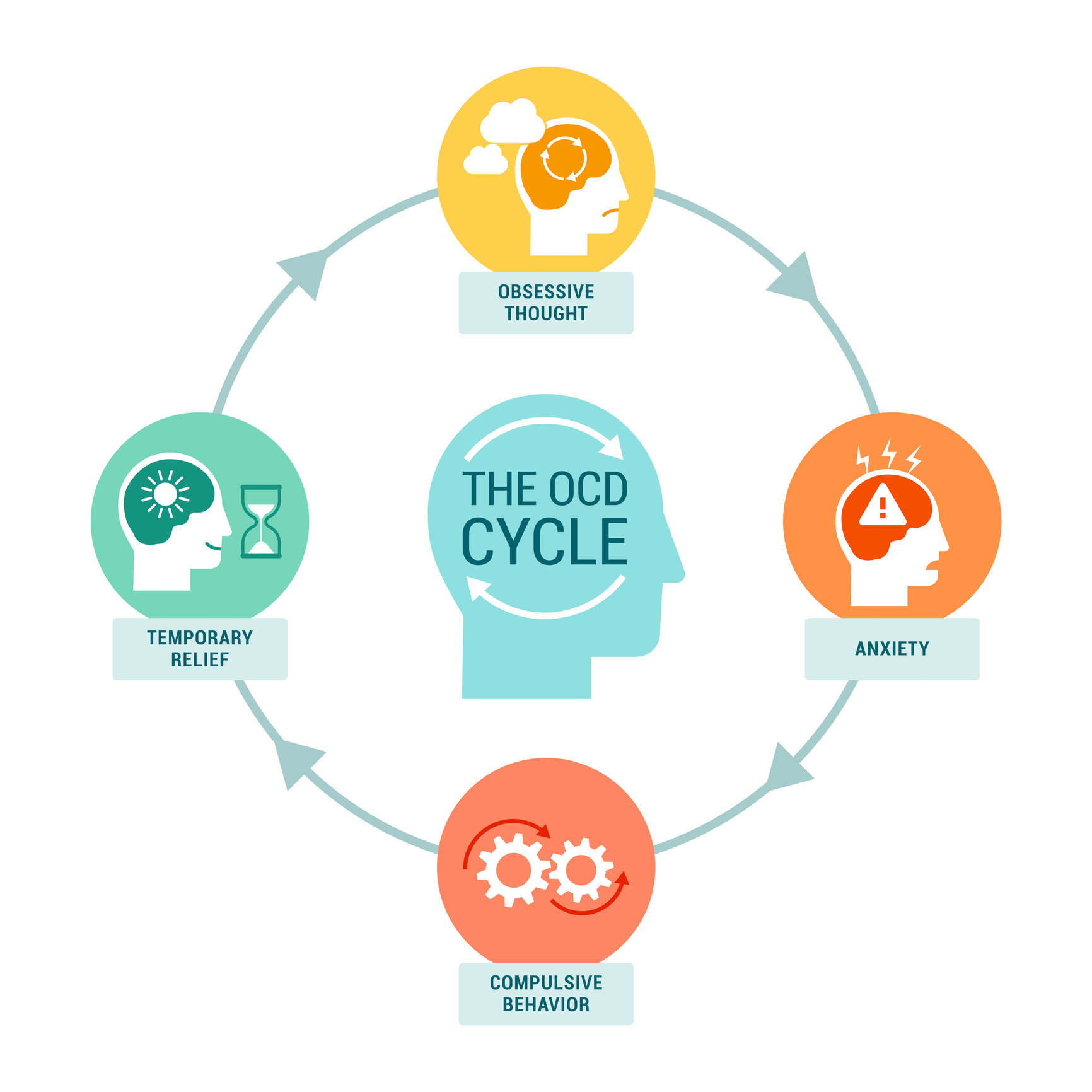
The OCD Obsessive Compulsive Disorder Cycle
The OCD cycle begins with the emergence of distressing obsessive thoughts, such as fears of contamination or doubts about safety. To alleviate this anxiety, individuals engage in compulsive behaviors, like washing their hands excessively or checking locks, reinforcing the belief that these actions are necessary, thus perpetuating the cycle of obsession and compulsion.

Additional Signs Of OCD
In addition to the common symptoms mentioned earlier, OCD can manifest in various ways, and individuals may experience a range of signs and behaviors associated with the disorder. Here are some additional signs of OCD:
- Mental Rituals: Some individuals with OCD engage in mental rituals, such as repeating certain phrases, silently counting, or mentally reviewing specific details to reduce anxiety related to their obsessions.
- Need for Reassurance: People with OCD often seek frequent reassurance from others to alleviate their doubts or concerns. They may repeatedly ask for confirmation or validation regarding their fears or actions.
- Avoidance: To prevent triggering their obsessions or the need to perform compulsions, individuals with OCD may go to great lengths to avoid certain situations, places, or objects that they associate with anxiety or distress.
- Intrusive Thoughts: These are unwanted and distressing thoughts that can range from violent or disturbing imagery to doubts about one's own morality or safety. Intrusive thoughts can be a hallmark of OCD.
- Ruminating: People with OCD may spend a significant amount of time ruminating or excessively thinking about their worries, often replaying scenarios in their minds to seek reassurance or certainty.
- Difficulty Concentrating: The constant presence of obsessive thoughts and the need to perform compulsions can make it challenging for individuals with OCD to concentrate on tasks, leading to reduced productivity and increased frustration.
- Emotional Distress: OCD can cause significant emotional distress, including anxiety, depression, guilt, shame, and frustration, as individuals grapple with their obsessions and compulsions.
- Impact on Relationships: OCD can strain relationships, as partners, family members, and friends may not fully understand the nature of the disorder or the need for rituals, leading to conflicts and misunderstandings.
- Impaired Functioning: In severe cases, OCD can impair a person's ability to perform everyday activities, maintain employment, or pursue personal goals due to the overwhelming impact of their obsessions and compulsions.
It's important to remember that OCD symptoms can vary widely from person to person, and not everyone with OCD will experience all of these signs. Additionally, the severity of symptoms can also vary, with some individuals having mild or moderate OCD and others experiencing more severe forms of the disorder. Seeking professional help from a mental health specialist is crucial for proper diagnosis and effective treatment.

What is the difference between OCD and OCPD - Obsessive Compulsive Personality Disorder
Obsessive-Compulsive Disorder (OCD) vs. Obsessive-Compulsive Personality Disorder (OCPD)
Nature:
- OCD: OCD is primarily an anxiety disorder characterized by the presence of obsessions and compulsions.
- OCPD: OCPD is a personality disorder characterized by a longstanding pattern of perfectionism, a preoccupation with rules and orderliness, and a need for control.
Obsessions:
- OCD: Individuals with OCD experience distressing, intrusive, and unwanted thoughts, images, or urges. These obsessions lead to intense anxiety or discomfort.
- OCPD: OCPD does not involve obsessions in the same way that OCD does. Instead, individuals with OCPD have a rigid preoccupation with rules and orderliness.
Compulsions:
- OCD: Compulsions are repetitive behaviors or mental acts performed in response to obsessions. These actions aim to reduce the anxiety or discomfort associated with the obsessions.
- OCPD: OCPD does not involve compulsions in the same way as OCD. Instead, individuals with OCPD exhibit perfectionistic behaviors and a need for control.
Insight:
- OCD: Most individuals with OCD are aware that their obsessions and compulsions are excessive or irrational. They often struggle to resist them but recognize their senselessness.
- OCPD: Individuals with OCPD typically do not see their behaviors as problematic. They believe their way of thinking and doing things is correct and may resist change or compromise.
Treatment:
- OCD: OCD is typically treated with cognitive-behavioral therapy (CBT), particularly Exposure and Response Prevention (ERP), and in some cases, medication like SSRIs.
- OCPD: OCPD is less responsive to traditional therapeutic approaches compared to OCD. Treatment may focus on improving interpersonal relationships and flexibility, but individuals with OCPD may be less willing to engage in treatment due to their perception that their behavior is appropriate.
In summary, OCD and OCPD, despite some similarities in terminology, are distinct conditions with different underlying features and treatment approaches. OCD involves anxiety-driven obsessions and compulsions, often accompanied by insight into their irrationality, while OCPD is characterized by rigid perfectionism, a need for control, and a lack of insight into the problematic nature of these traits.


What are the Best Treatments and Therapies for Obsessive Compulsive Disorder
Freedom from OCD!
Treatment for Obsessive-Compulsive Disorder (OCD) typically involves a combination of psychotherapy and, in some cases, medication. These treatments are effective in managing OCD symptoms by addressing the underlying causes and helping individuals regain control over their lives. Here are the primary treatments and therapies for OCD:
- Cognitive-Behavioral Therapy (CBT): CBT, particularly a specific form called Exposure and Response Prevention (ERP), is considered the gold standard for treating OCD. In ERP, individuals are gradually exposed to situations or triggers that provoke their obsessions while simultaneously preventing the usual compulsive responses. Over time, this exposure helps reduce anxiety and weaken the connection between obsessions and compulsions. CBT also includes cognitive restructuring, which helps individuals change their thought patterns and beliefs related to their obsessions.
- Medication: Selective Serotonin Reuptake Inhibitors (SSRIs) are commonly prescribed medications for OCD. These drugs, such as fluoxetine (Prozac) and sertraline (Zoloft), help regulate serotonin levels in the brain, which can reduce the intensity of obsessions and compulsions. For some individuals with severe OCD, combining SSRIs with CBT can be particularly effective.
- Psychodynamic Therapy: This type of therapy explores the underlying emotional and psychological factors that may contribute to OCD. Psychodynamic therapy can help individuals gain insight into their thoughts and behaviors, addressing deep-seated issues that may be fueling their OCD.
- Mindfulness-Based Therapies: Mindfulness techniques, such as Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), can help individuals with OCD develop greater awareness of their thoughts and feelings without judgment. Mindfulness can be used in conjunction with other therapies to reduce the distress caused by obsessions.
- Group Therapy: Group therapy sessions can provide individuals with OCD a supportive environment to share their experiences and learn from others. Group settings also offer opportunities for exposure exercises and practicing ERP techniques.
- Family Therapy: OCD can impact not only the individual but also their family members. Family therapy can help educate and involve family members in the treatment process, fostering better understanding and support for the person with OCD.
These treatments are effective for several reasons:
- Evidence-Based: Many of these treatments have been extensively researched and have a strong evidence base, demonstrating their effectiveness in reducing OCD symptoms.
- Targeting Root Causes: CBT, ERP, and psychodynamic therapy aim to address the root causes and triggers of OCD, helping individuals understand and manage their obsessions and compulsions.
- Medication Support: SSRIs can help balance brain chemistry, reducing the intensity of obsessions and compulsions, which can be particularly beneficial for individuals with severe OCD.
- Customized Approach: Treatment plans are often tailored to the individual's unique symptoms and needs, ensuring that they receive the most appropriate interventions.
- Long-Term Management: These treatments not only help alleviate symptoms but also equip individuals with strategies for long-term management of their OCD, promoting lasting recovery.
Overall, a combination of therapy and medication, along with ongoing support, offers individuals with OCD the best chance for significant symptom reduction and improved quality of life. Treatment success may vary from person to person, but with proper guidance and commitment, many individuals can effectively manage their OCD and lead fulfilling lives.
What about OCD In children? Cycle
Obsessive-Compulsive Disorder (OCD) can manifest in children much like it does in adults, but with some unique considerations. In children, OCD often begins subtly, and parents or caregivers may notice an increase in rituals or compulsive behaviors. Common obsessions in children with OCD can include fears of contamination, harm to loved ones, or worries about symmetry and order. These obsessions can lead to compulsions like excessive handwashing, checking locks, or arranging objects meticulously. OCD in children can significantly disrupt daily life, including school performance and social interactions. Early recognition and intervention, such as cognitive-behavioral therapy (CBT) tailored for children, is crucial to help them manage their symptoms effectively and minimize the impact of OCD on their development and well-being. OCD therapy for children can help!